Capture more high-value referrals with CoreCare Pre-Admit
Leverage AI for instant, expert-level referral reviews that improve competitiveness and grow revenue in fast-moving referral markets.
CoreCare is trusted by leading SNF operators across the country:
.png?width=200&height=110&name=Untitled%20design%20(7).png)
.png?width=200&height=110&name=Untitled%20design%20(18).png)
.png?width=200&height=110&name=Untitled%20design%20(8).png)
.png?width=200&height=110&name=Untitled%20design%20(9).png)
.png?width=200&height=110&name=Untitled%20design%20(19).png)
Win high value referrals
Win the best referrals with quick responses to referral partners - all without sacrificing quality and ensuring a low write-off risk.
Eliminate clinical review bottlenecks
When referrals linger in limbo, marketers lose opportunities. Our clinical screen instantly identifies red flags, diagnosis, and high cost medications.
Improve transparency
Track staff and facility performance, along with admissions trends for a full picture of your process, response times, and more.
How it works
.jpg?width=6008&height=4096&name=Document%20Scanning%20(2).jpg)
Document Scanning
CoreCare automatically collects all discharge paperwork and EHR data and feeds it to our AI agents responsible for financial verification, clinical verification, and medical necessity verification.
It's able to scan hundreds of pages of documentation in seconds, getting the right information, along with our insights, to the right person instantly.
.jpg?width=6008&height=4096&name=Financial%20Verification%20(1).jpg)
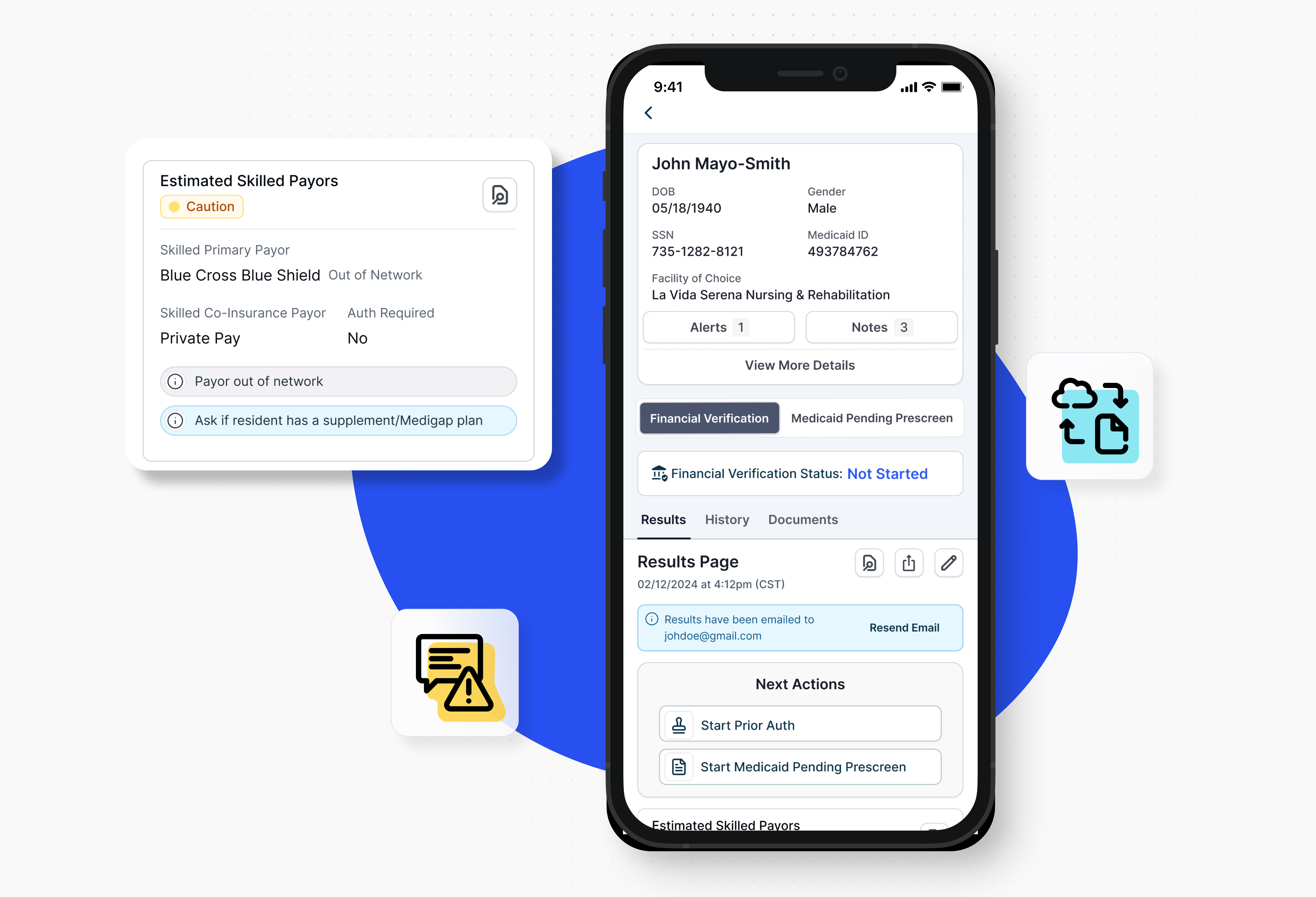
Financial Verification
CoreCare completes a comprehensive eligibility analysis on the prospective resident based on organization, state, and CMS rules and policies. SNF teams can:
- Obtain eligibility from Medicare, Medicaid and insurance plans
- Identify Skilled, Long-term Care and Therapy payers
- Identify a qualifying hospital stay or prior SNF stay
- In/out of Network results, SNF & plan specific benefits for Part C plans
- Medicaid pending pre-screen questionnaires
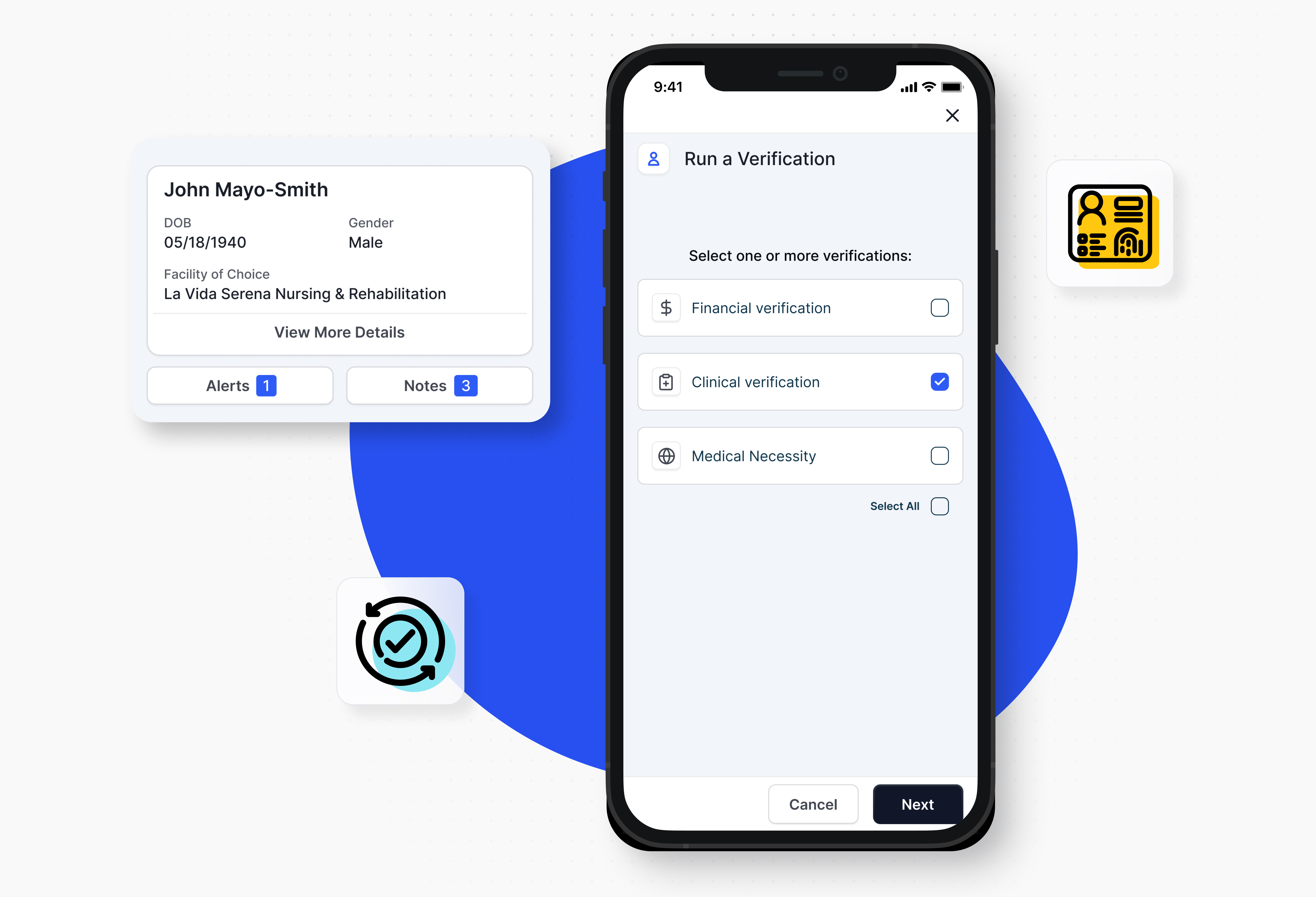
Clinical Verification
CoreCare performs a clinical verification, scanning all discharge paperwork and available EHR data to identify any issues that would be a red or yellow flag for the facility, including diagnosis, high cost medications, and any clinically relevant policies at your organization. Additionally, it checks to ensure the prospective resident is not on any sex offender registry.
Clinical Reimbursement Screen
CoreCare scans all discharge paperwork to estimate medical necessity for both Medicaid and Medicare. MDS nurses are delivered a copy of this report to ensure all necessary care is captured for the admissions MDS assessment.
Scoring
CoreCare compiles all of the data and issues for a Green/Yellow/Red decision. It also prepares a comprehensive PDF packet with all evidence, sending one copy to the team and another to your EHR.
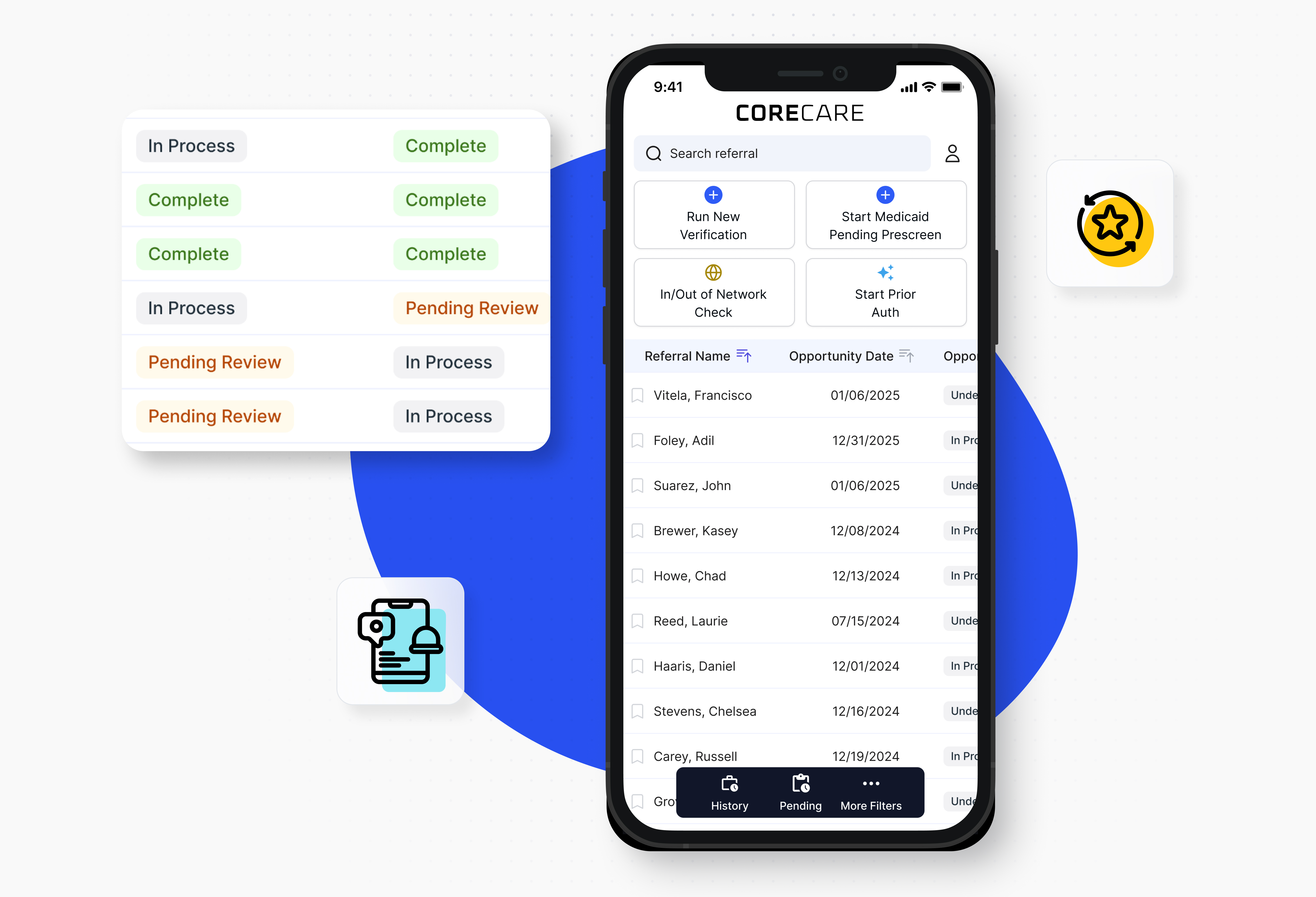
Explore CoreCare Pre-Admit Capabilities
We have all the tools you need for an effective admissions process
.png?width=1116&height=1572&name=Untitled%20design%20(21).png)
CRM
Capture and manage referrals, tracking their status through the admissions process, along with all their financial and clinical documentation.
Messaging
Keep families, referral partners, and your team informed about admission status, while leveraging a single platform to communicate internally.
Alerts, Prompts, and Next Steps
Customize your admissions process with alerts, prompts, and next steps, so every admission is conducted at an expert level, regardless of staff tenure or skill.
Analytics & Reporting
AI Agents
CoreCare scans and inputs medical and financial documents into the system, while surfacing key financial eligibility and clinical insights for your team.
Workflow Automation
CoreCare automates manual processes like Medicaid pending pre-screens, patient liability calculations, and more.
Schedule Demo
Are you interested in seeing CoreCare Pre-Admit in action? Fill out this form and someone from our team will get in touch to schedule a demo!
.png?width=250&height=75&name=CoreCare%20Logo%20(250%20x%2075%20px).png)